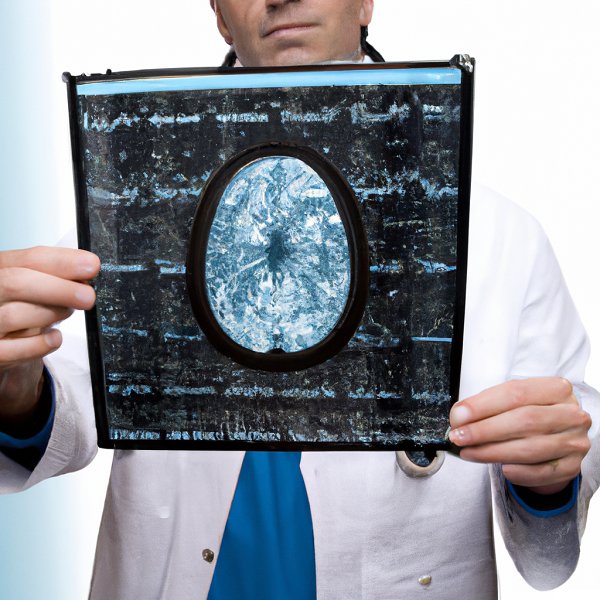
Differences in the working tissue of the brain, called grey matter, have been linked to impaired functioning of an emotion-regulating circuit in patients with borderline personality disorder.
People with borderline personality disorder (BPD) had excess grey matter in a fear hub deep in the brain, which over-activated when they viewed scary faces.
In contrast, the hub’s regulator near the front of the brain was deficient in grey matter and underactive, effectively taking the brakes off a runaway fear response, suggest researchers supported in part by NIMH.
These imaging studies are the first to link structural brain differences with functional impairment in the same sample of BPD patients. Similar changes in the same circuit have been implicated in mood and anxiety disorders, hinting that BPD might share common mechanisms with mental illnesses that have traditionally been viewed in a biological framework.
Michael Minzenberg, M.D., of theUniversity of California, Davis, and NIMH grantees Antonia S. New, M.D., and Larry J. Siever, M.D., of Mount Sinai School of Medicine, and colleagues, reported on their magnetic resonance imaging (MRI) findings in the July, 2008 issue of the Journal of Psychiatric Research. Their functional imaging findings were reported in the August 2007 issue of Psychiatric Research Neuroimaging.
Anger Depression and Anxiety
Accounting for up to 20% of psychiatric hospitalizations, BPD affects up to 1.4% of adults in a year. It is characterized by intense bouts of anger, depression, and anxiety that may last only hours, often in response to perceived rejection.
People with this difficult-to-treat disorder typically experience tumultuous work and family life and may engage in risky, impulsive behaviours. Cutting, burning and other forms of self-harm are common. The completed suicide rate in BPD approaches 10%, and at least 75% of afflicted individuals attempt suicide at least once.
Previous findings of lower-than-normal grey matter (neurons and their connections) in the regulator hub, called the anterior cingulate cortex (ACC), hinted that this might affect the way the brain works in BPD.
To investigate, the researchers first used functional magnetic resonance imaging (fMRI), to compare responses of 12 adult BPD patients with those of 12 healthy controls to pictures of faces with fearful, angry and neutral expressions.
In response to fearful faces, the amygdala, the fear hub, showed exaggerated activity in the BPD patients, while the ACC was relatively underactive. Since ACC activity would normally increase to dampen an overactive amygdala, this suggested weak regulation of emotion in the circuit.
Structural Brain Differences
Suspecting that this functional impairment mirrors structural differences, as has been found in depression, the researchers next used anatomical MRI to compare grey matter in the same patients and healthy controls.
Consistent with the fMRI results and the earlier findings, grey matter density was increased in parts of the amygdala and decreased in parts of the ACC, in BPD patients relative to controls. This suggested an abnormality in the number or architecture of neurons in these key components of the emotion-regulating circuit, which other evidence links to impaired functioning of the serotonin chemical messenger system.
While more research is needed on this subject it shows some interesting results and could well answer a few of the mysteries that surround BPD.